Snakebites remain one of the world’s most neglected tropical diseases, claiming an estimated 81,000 to 138,000 lives each year and leaving hundreds of thousands more with permanent disabilities, according to the World Health Organization. In rural areas of Africa, Asia, and Latin America, where access to medical care is limited, a single bite from a venomous snake can spell disaster. Traditional antivenoms, derived from horse or sheep serum, are often species-specific, expensive to produce, and prone to causing allergic reactions. But in a groundbreaking study published in May 2025, scientists have harnessed human antibodies to create the broadest antivenom yet one that neutralizes neurotoxins from 19 of the deadliest elapid snakes, offering hope for a more effective, safer treatment.
The story begins with Timothy Friede, a Wisconsin truck mechanic and herpetology enthusiast who, over 18 years, deliberately exposed himself to venom from hundreds of snakebites and injections 856 times in total. His goal? To build personal immunity against accidental bites from his pet snakes. While extremely dangerous and not recommended, Friede’s hyperimmune blood became a treasure trove for researchers at Centivax and Columbia University. By isolating DNA from his B cells, they created a library of over a billion antibodies, screening them for those that could bind and neutralize key snake neurotoxins.
This approach marks a shift from conventional antivenom production, which involves immunizing animals with venom, harvesting their antibodies, and purifying them a process that’s costly, variable in quality, and limited in scope. Human-derived antibodies, produced recombinantly, promise greater consistency, reduced side effects, and scalability.
What Are Snake Neurotoxins?
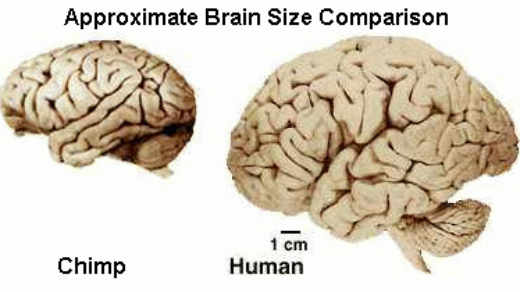
Elapid snakes, which make up about half of all venomous species, include notorious predators like cobras, mambas, kraits, taipans, and coral snakes. Their venoms primarily contain neurotoxins that target the nervous system, leading to paralysis, respiratory failure, and death if untreated. The key culprits are alpha-neurotoxins, part of the three-finger toxin (3FTx) family. These small proteins fold into a distinctive “three-finger” shape and bind tightly to nicotinic acetylcholine receptors (nAChRs) at neuromuscular junctions, blocking nerve signals to muscles.
3FTx come in two main varieties: long-chain (66-74 amino acids, binding strongly to muscle nAChRs) and short-chain (60-62 amino acids, with broader but weaker binding). Many elapids also produce secretory phospholipase A2 (sPLA2) enzymes, which can enhance neurotoxicity by damaging nerve terminals or causing inflammation. The diversity of these toxins across species has long hindered broad-spectrum antivenoms, as antibodies effective against one snake’s venom may fail against another’s.
Mixing the Ultimate Antivenom
From Friede’s antibody library, researchers identified two standout broadly neutralizing antibodies: LNX-D09 and SNX-B03. LNX-D09 excels at neutralizing long-chain 3FTx from species like cobras and mambas, while SNX-B03 targets short-chain variants more effectively. Crystal structures of these antibodies bound to toxins reveal a clever mechanism: they mimic the structure of nAChRs, binding to conserved epitopes on the toxins’ receptor-interacting loops. This “mimicry” prevents the toxins from latching onto real receptors, effectively disarming them.
To broaden coverage, the team added varespladib, a small-molecule inhibitor already in clinical trials for other uses. Varespladib potently blocks sPLA2 enzymes, addressing toxins that the antibodies alone couldn’t fully neutralize. This three-component cocktail wo antibodies plus varespladib was tested in mice challenged with lethal doses of whole venom from 19 elapid species classified as WHO Category 1 (highest medical importance) or Category 2 (secondary importance).
The World’s 19 Deadliest Killer
The panel included snakes from across Africa, Asia, Australia, and the Americas, selected for their high bite incidence and lethality. Key species encompass African mambas (black mamba, eastern green mamba, Jameson’s mamba, western green mamba), cobras (king cobra, Indian cobra, Cape cobra, Philippine cobra, black-necked spitting cobra), kraits (common krait, many-banded krait), taipans (inland taipan, coastal taipan), and other elapids including tiger snake, eastern coral snake, and death adders.

These snakes are responsible for a significant portion of global snakebite morbidity, with neurotoxic effects causing rapid paralysis. The WHO lists them based on factors like venom potency, bite frequency, and human proximity.
Venom Mix Saves Mice from 13 Killer Snakes
In vivo tests were rigorous: Mice received lethal venom doses, followed by the antivenom cocktail with up to a 10-minute delay to simulate real-world scenarios. Results were impressive, with full protection (100% survival) achieved for 13 species, including black mamba, king cobra, four cobra species, inland taipan, and common krait. Even with delayed administration, symptoms like paralysis were prevented. Partial protection (delayed onset or reduced severity) was observed in the remaining six species, such as some death adders and tiger snakes, where survival rates improved but weren’t complete.
LNX-D09 alone protected against six species, SNX-B03 extended coverage, and varespladib filled gaps for sPLA2-dominant venoms. No local tissue damage or hemorrhage was noted, focusing solely on neurotoxin neutralization.
Implications and Future Directions
This antivenom represents a major step toward a “universal” treatment, potentially revolutionizing care in snakebite hotspots. Human antibodies minimize allergic risks compared to animal-derived ones, and recombinant production could lower costs and improve shelf-life no refrigeration needed. However, it targets only elapids’ neurotoxins; viperid snakes, with their hemotoxic venoms, require separate solutions. Clinical trials in humans are next, along with optimizing dosing and combining with viper antivenoms for pan-family coverage.
Before this breakthrough antivenom can reach patients in remote villages and clinics, several critical steps remain. Human clinical trials must establish safety profiles, appropriate dosing regimens, and efficacy across diverse populations. Researchers will need to determine optimal administration protocols, including whether the treatment can be given by minimally trained healthcare workers in field settings where snakebites most commonly occur.
Manufacturing and Distribution Challenges
Scaling up production of recombinant human antibodies presents both opportunities and obstacles. Unlike traditional antivenoms that require maintaining herds of immunized horses or sheep, recombinant production uses cell culture systems that can be standardized and replicated globally. This could dramatically reduce costs and ensure consistent quality. The stability of these antibodies at room temperature could eliminate the “cold chain” problem that has plagued antivenom distribution in tropical regions where refrigeration is unreliable.
Economic Impact on Snakebite Burden
The financial toll of snakebites extends far beyond immediate medical costs. Victims often face long-term disabilities, lost wages, and impoverishment. In agricultural communities where snakebites are most prevalent, a single breadwinner’s injury can devastate an entire family. An affordable, effective antivenom could prevent an estimated $2.5 billion in annual economic losses across affected regions, according to health economists studying tropical disease burden.
Addressing the Viper Gap
While this antivenom marks tremendous progress for elapid bites, vipers and pit vipers remain a significant threat, particularly in the Americas and parts of Asia. These snakes employ hemotoxic venoms that cause tissue destruction, internal bleeding, and organ failure through different mechanisms than neurotoxins. Researchers are already exploring whether similar antibody-discovery approaches could identify broadly neutralizing antibodies against viper toxins, particularly the metalloproteinases and serine proteases responsible for hemorrhagic effects.
Lessons from a Snakebite Self-Experimenter’s Survival
Timothy Friede’s unconventional path to immunity raises important ethical questions about citizen science and self-experimentation. While his contribution proved invaluable, medical ethicists emphasize that his approach was extraordinarily dangerous and could have easily resulted in his death or permanent disability. The case highlights a tension between individual autonomy and responsible medical practice, as well as the unexpected ways scientific breakthroughs can emerge from unorthodox sources.
Friede’s hyperimmune status demonstrates that the human immune system, given sufficient exposure, can generate antibodies capable of neutralizing even the most potent natural toxins. This principle is now being applied to other medical challenges, from emerging infectious diseases to cancer immunotherapy. The antibody library approach creating vast collections of human antibodies and screening them for desired properties has become a cornerstone of modern therapeutics development.
In 2019, the World Health Organization launched a roadmap to halve snakebite deaths and disabilities by 2030. This new antivenom aligns perfectly with that goal, offering a potential game-changer for the world’s poorest communities. However, success depends on ensuring equitable access. History shows that medical innovations often remain out of reach for those who need them most due to cost, distribution barriers, or lack of awareness.
Even the most effective antivenom cannot address the full scope of the snakebite crisis. Prevention through education, protective equipment for agricultural workers, and improved housing to reduce snake-human encounters must remain priorities. Communities need training to recognize dangerous species, administer first aid, and seek appropriate medical care quickly since even the best antivenoms work best when given promptly.
The Future of Toxin Research
The techniques developed for this antivenom have broader applications. Scorpion stings, jellyfish venom, and spider bites cause similar public health burdens in different regions. The antibody-discovery platform used here could be adapted to create treatments for these envenomations as well. Some researchers are even exploring whether modified versions of venom-neutralizing antibodies might have therapeutic uses, as venom components sometimes inspire drug development.
Looking further ahead, synthetic biology approaches could enable on-demand production of antivenoms tailored to specific geographic regions or even individual patients. CRISPR-based technologies might allow rapid modification of antibodies to improve their binding or extend their coverage. Some envision a future where portable devices could diagnose the specific snake species involved in a bite and dispense a customized antivenom cocktail on the spot.
Modern Chapter in Snakebite Medicine
In a world where snakebites disproportionately affect the poor and marginalized, this innovation could save countless lives and prevent untold suffering. As lead researcher Jacob Glanville notes, “We had dramatically unparalleled breadth of protection.” The journey from a daring individual’s blood to a life-saving cocktail underscores the power of unconventional science in tackling global health challenges.
The development of this broad-spectrum antivenom represents more than just a scientific achievement it embodies hope for communities that have long been overlooked by modern medicine. While challenges remain in bringing this treatment from laboratory to bedside, particularly in the remote areas where it’s needed most, the progress made demonstrates that even the world’s most neglected diseases can yield to human ingenuity and determination.
As clinical trials move forward and production scales up, the global health community watches with cautious optimism. If successful, this antivenom won’t just save individual lives it will validate a new approach to therapeutic development that could transform how we address toxic threats across the natural world. For the subsistence farmers, rural workers, and vulnerable children who live with the daily threat of snakebite, that transformation cannot come soon enough.
Reference:
Cell Press. Antivenom neutralizes the neurotoxins of 19 of the world’s deadliest snakes.