Prosopometamorphopsia is neurological disorders causes people to see monsters. It distorts how people perceive human faces that twisting familiar features into terrifying shapes. A Dutch woman’s lifelong struggle with this condition not only target the personal toll on the other hand, provides medical researchers with valuable clues about how the brain processes vision and identity.
What Are Prosopometamorphopsia Dragon Hallucinations?
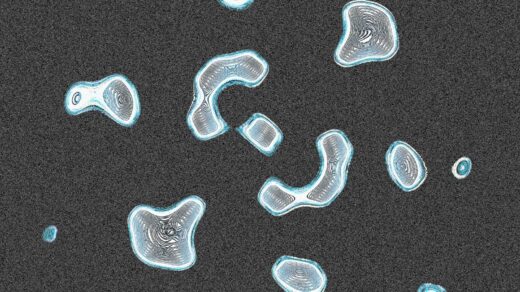
For more than 40 years, a 52-year-old woman from The Hague lived in terror. Every face she saw shifted into something monstrous like a devil. Eyes glowed in vivid yellows, blues, or reds. Skin turned black and reptilian. Ears stretched into long, pointed shapes. Noses and mouths jutted outward until the entire face resembled a dragon.
These terrifying distortions were not limited to social interactions. Even when she was completely alone in at a place dragon faces would materialize in front of her. For decades, she avoided gatherings, struggled to work, and lived under a constant shadow of fear.
The Long Road to Diagnosis
After years of isolation, she finally sought help at a psychiatric clinic. Standard tests brought no answers. Her blood work appeared normal. EEG scans did not show unusual brain activity also neurological exams revealed no obvious problems seemed alright.
It was not until doctors performed an MRI that they discovered a clue. Several small lesions appeared around the lentiform nucleus, deep in the brain’s white matter. This white matter acts like the communication network of the brain, connecting regions that handle vision, memory, and recognition. Doctors suspected the lesions disrupted signals in the ventral occipitotemporal cortex which is a small region essential for face recognition.
What Is Prosopometamorphopsia?
Doctors concluded that the woman was living with prosopometamorphopsia (PMO). This condition alters the way faces are perceived. Unlike prosopagnosia, which makes it hard to recognize faces, PMO warps how faces physically appear.
Symptoms vary widely. Some patients see faces that are stretched, sagging, or discolored. Others describe features that drift out of place or resemble grotesque masks. A few, like this Dutch woman, experience visions so vivid they seem almost hallucinatory.
What makes her case extraordinary is its duration. While PMO typically lasts only days or weeks, she had lived with the condition since childhood. Medical literature has documented fewer than 100 cases worldwide, making her situation exceptionally rare.
Her first treatment was valproic acid, a medication often used for seizures and migraines. The results were promising: her dragon-like visions faded for the first time in decades. But soon another problem surfaced—loud banging sounds that echoed in her mind whenever she tried to sleep.
To ease these new auditory hallucinations, her doctors prescribed rivastigmine, a drug more commonly used in Alzheimer’s and Parkinson’s patients. This change worked better. The banging sounds became rare, and the visual distortions dropped to a manageable level.
Three years later, her life looked dramatically different. She could keep a stable job. She could meet friends without overwhelming fear. While some symptoms remained, they no longer controlled her daily existence.
Why This Case Matters
Her story provides more than personal relief. It offers into how the brain processes the most familiar image we see the human face. By studying how lesions in the brain’s wiring altered her perception doctors gained clues about the links between brain structure, electrical activity, and visual recognition.
The dragon like quality of her visions remains unexplained. Still, her case suggests that rare neurological disorders may hold answers to broader medical mysteries. Each patient with prosopometamorphopsia helps expand scientific understanding of how we see and recognize one another with the help of our neurons.
The Dutch woman’s journey proves that even after decades of suffering effective treatments can be found. Her transformation from isolation to connection shows the importance of seeking medical help, even for symptoms that seem impossible to describe.
For researchers, her case is a reminder that rare conditions can illuminate hidden corners of the human brain. For patients, it provides hope that unusual struggles may eventually find explanation and relief.
The information in this article is intended for educational use only and does not substitute professional medical guidance.
RathBiotaClan