Artificial womb technology is no longer just science fiction. A viral hoax about a $14,000 pregnancy robot from China stirred up debate, but behind the fake headlines lies a very real and growing field of research. So, how close are we to creating real artificial wombs and what challenges stand in the way?
Recently, it latched on to a story about a supposed “$14,000 pregnancy robot from China.” The tale spread fast across social media. It featured images of shiny chrome robots with wiring visible, each carrying plump human babies inside transparent bellies. At the center of the reports was a man named Zhang Qifeng. He was described in conflicting ways—sometimes as the CEO of Guangzhou-based Kaiwa Technology, other times as a PhD graduate of Singapore’s Nanyang Technological University (NTU). Zhang allegedly promised a working prototype by 2026, priced under 100,000 yuan (around $13,900). He claimed the robot would allow people to have children without marriage or the hardships of pregnancy.
But there was one big problem: none of it was true.
Fact-checkers at Live Science and Snopes quickly debunked the story. There is no Kaiwa Technology. NTU confirmed no PhD graduate named Zhang Qifeng is working on such research. No evidence existed of the so-called pregnancy bots. Still, the hoax managed to spark serious discussion about artificial wombs—what’s real, what’s possible, and what remains pure science fiction.
Where science actually stands: Artificial wombs for premature babies
While a full pregnancy robot is fantasy for now, real scientists are actively developing artificial womb-like systems but for a very different purpose. At the Children’s Hospital of Philadelphia (CHOP), researchers are working on EXTEND (extra-uterine environment for newborn development).
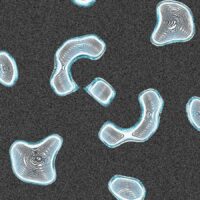
The goal isn’t to grow babies from scratch. It’s to help extremely premature infants, those born between 23 and 28 weeks of gestation. These tiny babies face high risks of chronic lung disease, brain development problems, and death. EXTEND uses a sealed bag filled with lab-made amniotic fluid rich in nutrients and growth factors. An external oxygenator acts like a partial placenta, exchanging oxygen and carbon dioxide. The system shields the baby from dangerous shifts in light, temperature, pressure, and exposure to germs.
Results in animal testing look promising. Lambs supported in EXTEND for about a month continued normal development, including preserved brain gene activity. Human trials are expected. However, scientists caution that current neonatal intensive care technology already helps many premature survive. So, ethics and medical necessity will be key to be deciding how and when to test this method.
As Dr. Lusine Aghajanova from Stanford Medicine said, it’s a concept that can work, but it’s “more complicated than we think.” BTW; EXTEND is not designed to replace pregnancy from conception to birth. It acts only as a temporary bridge for premature babies.
Why a full “pregnancy robot” is almost impossible today
To go from embryo to full baby in a machine would mean solving some extreme biological and engineering challenges. Experts highlight several almost impossible hurdles:
Implantation: The embryo must attach to uterine tissue to begin pregnancy. Dr. Harvey Kliman of Yale suggests a “hydroponics” approach suspending the embryo in fluid without attachment. But Dr. Aghajanova disagrees, stressing that implantation is critical, like “the seed and the soil.” Without it, normal placental and fetal development could fail.
Oxygen and nutrient control: Early pregnancy requires a low-oxygen environment to protect DNA. Later, it shifts to high oxygen as the fetus grows. A machine would need to reproduce this delicate transition perfectly. It must constantly adjust to changing metabolic demands.
Infection risks: Keeping a fetus free from infection for nine months in a complex artificial system is, as Kliman says, “the biggest problem.”
Immune system support: In the womb, mothers pass antibodies through the umbilical cord. A robot need to simulate this possibly with donated blood or synthetic antibodies. But the protective maternal immune role is still irreplaceable.
Microbiome influence: Babies also benefit from exposure to the vaginal microbiome, which shapes long-term health. Replicating this, when we still don’t fully understand it is another roadblock.
Material safety: Aghajanova warns that plastics or synthetic parts in a robot might disrupt development in unpredictable ways.
THE UNASWERED QUESTIONS !
Even if someone built a prototype, the unanswered questions are staggering.
Where would the eggs and sperm come from?
Would fertilization happen inside the machine or via IVF?
How would the birth process work?
Who regulates and tests such a device ethically?
What if babies raised this way missed unknown benefits of natural pregnancy?
The viral robot story was fake. But it highlighted how people are fascinated by the idea of “outsource” pregnancy. The reality is that science is nowhere close to gestating babies in machines. As Kliman said, it mostly shows “what a miracle a pregnancy is.” Natural gestation, despite its risks, remains far more reliable than anything technology that can deliver.
In countries like the U.S., where fertility treatments, egg/sperm donation, and surrogacy are already available. Experts agree that we aren’t desperate for pregnancy robots.
What we are doing instead is making steady, careful progress in saving premature babies. And that is where artificial womb technology really matters.
The information provided in this article is for educational purposes only and does not substitute professional medical guidance.
RathBiotaClan