In a recent study published in Translational Psychiatry, researchers investigated the association of viral RNAs in the choroid plexus (CP) with bipolar disorder (BPD) and schizophrenia (SCZ), provides evidence for the involvement of the Hepatitis C Virus (HCV) in neuropathology.
Background and Hypothesis
Epidemiological studies have long suggested a link between infectious agents, particularly viruses, and psychiatric disorders like schizophrenia and bipolar disorder. However, direct evidence of active viral infection in the brain associated with these conditions has been elusive, possibly because viruses may prefer to infect neuro-epithelium rather than neural tissue itself. The choroid plexus which forms the blood-cerebrospinal fluid barrier and protects the brain, was hypothesized as a likely site for viral infections due to its role as a filtration system and its known tropism for viruses. Neuroinflammation is consistently linked to psychiatric disorders, particularly schizophrenia, with evidences pointing to involvement of brain endothelial cells in these inflammatory changes.
Methodology
To test their hypothesis, the researchers employed viral sequence enrichment technology and RNA sequencing on postmortem choroid plexus (CP) samples from 84 individuals with schizophrenia (SCZ), 73 with bipolar disorder (BPD), 23 with major depression (MDD), and 76 unaffected controls, all from the Stanley Medical Research Institute brain collection.
This advanced technique allowed for the sensitive detection of hundreds of human and animal viral sequences, overcoming previous limitations in detecting low-copy-number latent viruses.
They also analyzed the TriNetX electronic health record database, encompassing over 285 million patients, to assess the prevalence of chronic HCV in these psychiatric populations. Furthermore, hippocampus RNA sequencing data from HCV-positive subjects were analyzed to determine if HCV RNA in the CP was associated with host transcriptional changes in the brain. HCV sequencing results were also confirmed using quantitative PCR (qPCR).
Key Findings
Overall Viral Detection in CP
The study identified the presence of 13 viral species in the CP of 46 subjects. CP samples from individuals with SCZ and BPD were more likely to contain viral sequences. Viruses were detected 52 times in 256 samples in this study, which is notably higher than a previous large assay of viral sequences in brain tissue that found viruses 48 times in 589 samples, suggesting the CP is a more prominent reservoir for viruses than neural tissue.
HCV Association
Among the identified viruses, Hepatitis C Virus (HCV) was the only viral species that reached statistical significance for an association with SCZ and BPD. While other viruses like Parvovirus B19, HHV-4, and HHV-7 were found in psychiatric cases but not controls, their sample numbers were too low to establish a definitive association.
Prevalence of Chronic HCV
Analysis of the TriNetX database confirmed a significantly higher prevalence of chronic HCV in SCZ (3.6%) and BPD (3.9%) populations, almost double that observed for MDD (1.8%) and approximately 7-fold higher than in the control population (0.5%). This finding challenges the assumption that the higher prevalence of HCV in SCZ and BPD is solely due to behaviors like intravenous drug use, as such behaviors are also present in MDD patients, where the prevalence was lower.
HCV Presence in CP vs. Brain Tissue
While HCV RNA was detected in the CP, it was consistently absent in the hippocampus of the same individuals. This suggests that HCV infection of the CP does not necessarily lead to direct infection of the brain. This finding is consistent with previous research indicating that HCV receptors are primarily found in neuroepithelial cells, and HCV is rarely detected in brain tissue.
Impact on Hippocampal Transcriptome
Despite of the absence of the virus in the hippocampus, the presence of HCV RNA in the CP was associated with robust and consistent host transcriptional changes in the hippocampus. These changes included alterations in the expression of 14 genes and a highly specific silencing of 185 repetitive elements, particularly Alu and L1 elements. These transcriptional changes are potentially related to the innate immune response activated by the virus or inflammation associated with the CP infection.
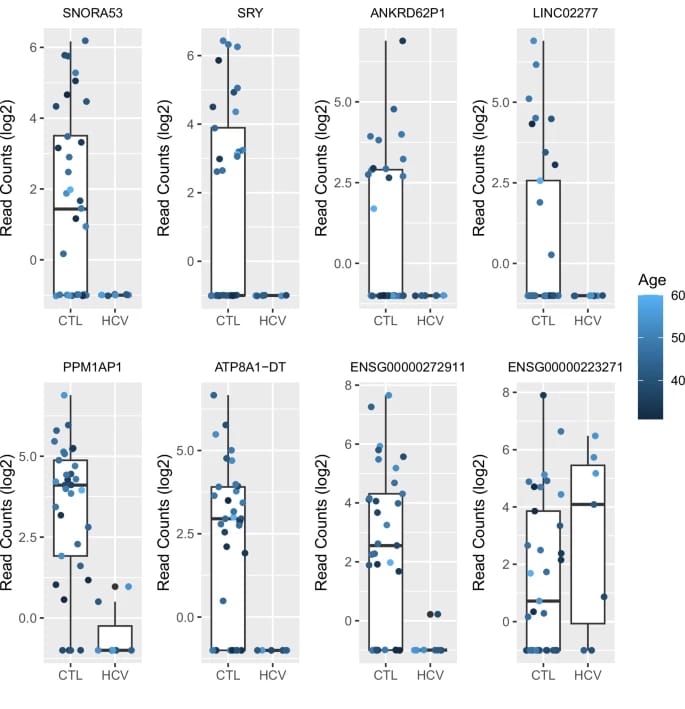
Figure 1.
Hippocampal gene expression alterations linked to HCV presence in the choroid plexus.
Boxplots display log2-transformed read counts of selected genes in the hippocampus, comparing individuals with (HCV) and without (CTL) HCV RNA detected in their choroid plexus. Each dot represents an individual, colored by age. Multiple genes, including SNORA53, SRY, and PPM1AP1, show reduced expression in the HCV group, highlighting downstream transcriptional effects in the brain despite the virus not being directly present in hippocampal tissue.
(Credit: Nature)
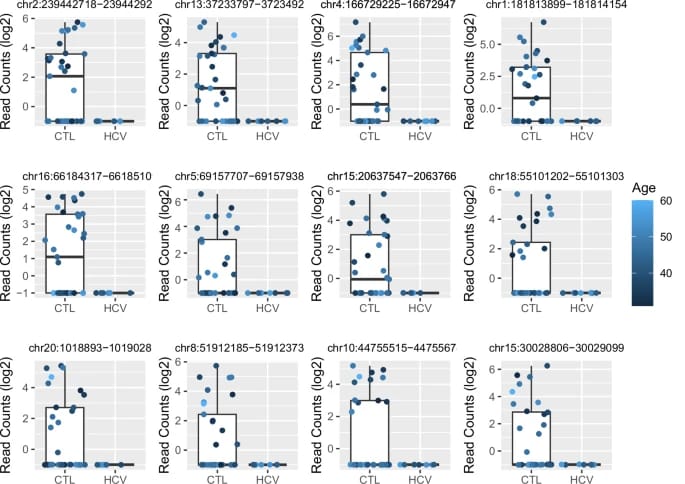
Figure 2.
Suppression of repetitive element expression in the hippocampus of individuals with HCV in the choroid plexus.
Log2 read count boxplots for selected repetitive genomic regions (identified by chromosomal coordinates) show a marked reduction in expression among HCV-positive individuals compared to controls. This widespread silencing, particularly of transposable elements such as Alu and LINE-1, suggests possible innate immune activation or epigenetic reprogramming in response to peripheral HCV infection.
(Credit: Nature)
Conclusions and Implications
The findings provide compelling support for the viral hypothesis of psychiatric disease, identifying HCV as a feasible viral pathogen contributing to the neuropathology of SCZ and BPD in a subset of patients. The choroid plexus appears to be a crucial reservoir for viruses, and targeting neuroepithelial structures like the CP could reveal further associations between infections and neural/psychiatric disorders.
The study emphasizes that the impact of HCV infection may extend beyond the liver, affecting cognitive and psychiatric functions. Given the demonstrated higher prevalence of HCV in SCZ and BPD, the authors underscore the guidance on universal HCV screening and treatment in SCZ and BPD patients as part of standard psychiatric care. They suggest that early treatment of HCV infection could potentially alleviate psychiatric symptoms and improve brain function, although further extensive investigation into its effectiveness for SCZ and BPD symptoms is needed. Future research aims to study the association of viruses in the cerebrospinal fluid (CSF) with SCZ and BPD, potentially leading to virus-specific biomarkers for CP infection and identifying patients who might benefit from HCV treatment.
Reference
NATURE – Translational Psychiatry